Analysis of the Department of Health & Social Care’s latest Health Trends data for England highlights record prevalence of serious health conditions.
The analysis from Broadstone, a leading independent consultancy, shows that cancerous issues have become significantly more common, with the proportion of patients with cancer (excluding non-melanotic skin cancers) more than doubling in just over a decade.
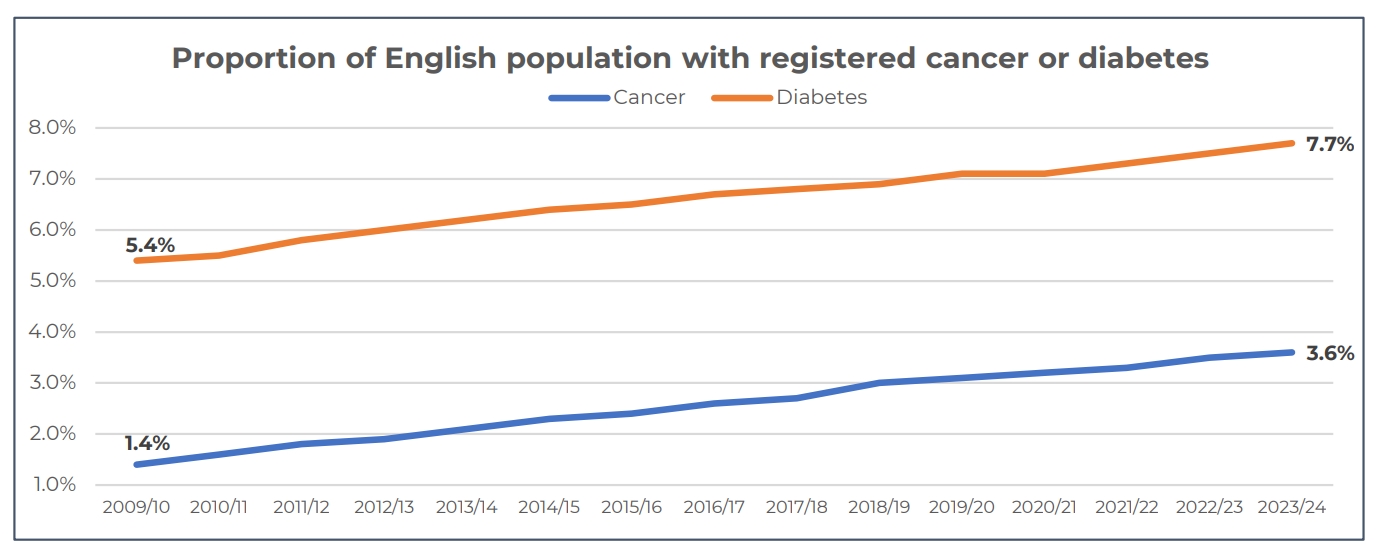
When records began in 2009/10, 1.4% of people in England – or 776,000 – had diagnosed cancer (excluding non-melanotic skin cancers) according to practice disease registers. This doubled to 3% in 2018/19 and has subsequently increased to 3.6% or 2.3 million in 2023/24 – the latest financial year.
It follows the latest ONS cancer waiting time statistics2 for England which showed that the percentage of patients waiting longer than the 62-day standard and 31-day standard for cancer treatment in England has more than tripled over the past 12 years.
In the second quarter of 2024, 33.4% were waiting longer than the 62-day standard, compared with 11.0% in Q1 2012. There should be no more than 62 days between a cancer referral being received by a hospital (specialist) to when a patient starts treatment.
In Q2 2024, 8.9% of patients were waiting longer than the 31-day standard for treatment, compared with just 1.6% in Q1 2012. There should be no more than 31 days from the “decision-to-treat” a cancer patient to when the patient starts treatment.
For cardiovascular risks, diabetes prevalence increased to a record 7.7% in 2023/24, a significant rise from 6.9% in 2018/19, and from 5.4% in 2009/10 when records began.
Among all ages, stroke, high blood pressure, and heart failure prevalence also hit record high levels in the latest financial year, with heart failure seeing the most significant increases in the last 10 years.
In 2009/10, the proportion of people with recorded heart failure stood at 0.72%, this has now increased significantly to 1.06% in 2023/24.
Brett Hill, Head of Health & Protection at Broadstone, said the data underscores the value of embedding ‘prevention’ at the heart of employee benefit programmes: “It’s deeply concerning to see the increasing prevalence of chronic, life-threatening conditions such as cancer, heart disease, and diabetes.
“While various factors contribute to these rising numbers, they coincide with lengthening NHS waiting lists and reduced access to timely primary care, issues that have worsened since the pandemic.
“Early detection and treatment are crucial, but with the NHS under immense strain, many cases go undiagnosed and untreated, leaving people at greater risk.
“In response, employers are increasingly focusing on preventative health strategies, such as comprehensive Private Medical Insurance, private GP services, and regular health screenings. These proactive measures not only protect employee health but also help reduce the long-term costs of healthcare by preventing more serious conditions from developing.”



